Q. What is Uterine Fibroid Embolization?
 A. Uterine Fibroid Embolization (UFE) is a procedure used to shrink and ultimately eliminate the symptoms many women experience from fibroids. Fibroids are benign (non-cancerous) tumors that develop in the muscular wall of the uterus. While fibroids do not always cause symptoms, their size and location can often cause women to experience heavy menstrual bleeding, pelvic pain and pressure, pain in the back or legs, pain during sexual intercourse, bladder pressure leading to a constant urge to urinate, or an abnormally enlarged abdomen.
A. Uterine Fibroid Embolization (UFE) is a procedure used to shrink and ultimately eliminate the symptoms many women experience from fibroids. Fibroids are benign (non-cancerous) tumors that develop in the muscular wall of the uterus. While fibroids do not always cause symptoms, their size and location can often cause women to experience heavy menstrual bleeding, pelvic pain and pressure, pain in the back or legs, pain during sexual intercourse, bladder pressure leading to a constant urge to urinate, or an abnormally enlarged abdomen.
UFE is a minimally invasive procedure that relieves the symptoms caused by fibroids in 97%
of the patients. Although there are other accepted treatments for fibroids, UFE is considered one of the least invasive procedures with generally little or no side effects to the patient.
Q. What is an Interventional Radiologist and why doesn’t my gynecologist offer this procedure?
A. Interventional Radiology is a rapidly growing area of medicine. Interventional Radiologists are specially trained doctors who use their expertise in reading x rays, ultrasound, and other medical images to guide small instruments through blood vessels and other pathways to treat disease without an open surgical incision. Most of all procedures performed by  Interventional Radiologists are minimally invasive (that is they do not require an open surgical incision) and are performed using imaging guidance (x-ray fluoroscopy, CAT scan, ultrasound, and/or MRI). The procedures performed by an Interventional Radiologist are typically less invasive and much less costly than traditional surgery. Interventional Radiologists are specially trained in performing these procedures.
Interventional Radiologists are minimally invasive (that is they do not require an open surgical incision) and are performed using imaging guidance (x-ray fluoroscopy, CAT scan, ultrasound, and/or MRI). The procedures performed by an Interventional Radiologist are typically less invasive and much less costly than traditional surgery. Interventional Radiologists are specially trained in performing these procedures.
While gynecologists are specially trained to performed hysterectomies, myomectomies and other less invasive laparoscopic and hysteroscopic surgical procedures, most of them have not been formally trained and therefore do not possess the skills necessary to perform uterine fibroid embolization.
Q. How are fibroids diagnosed?
A. Since a large majority of patients with fibroids are completely asymptomatic. The diagnosis is usually confirmed using ultrasound or less commonly MRI. In general, MRI is better than ultrasound in determining the exact size, number and location of the fibroids. It also provides information concerning the blood supply to the fibroids that ultrasound cannot provides.
Q. What are basic symptoms of fibroids?
A. Fibroid symptoms can be grouped into abnormal bleeding, pelvic pain, and those caused by mass effect by the enlarged uterus (bulk-type symptoms). Women may develop one or more of the following symptoms:
Abnormal bleeding - sub mucous and intramural fibroids can both cause menorrhagia (prolonged and/or profuse menstrual bleeding) sometimes leading to severe anemia. Gushing, or flooding, and passage of large clots can occur. In some cases there can be bleeding between periods (metrorrhagia).
Pelvic pain - typically associated with heavy menstrual flow with cramping (dysmenorrheal)
Bulk-type symptoms - those caused by individual fibroids, or the enlarged uterus, compressing adjacent structures.
Q. What are Treatment options for fibroids?
A. The most appropriate treatment for uterine fibroids depends on the severity and type of symptoms, size, number, and location of fibroids. Treatment options include:
Medications - usually tried first for patients with symptoms, especially those with abnormal bleeding.
Uterine Fibroid Embolization (UFE) - Medical therapy fails to control symptoms in up to 2/3 patients with abnormal bleeding and a higher percentage in those with bulk type symptoms. A now well established alternative to surgical therapy is uterine fibroid embolization. Using imaging guided angiographic techniques an Interventional Radiolgist blocks (embolizes) the blood supply to the fibroids which shrink, causing the symptoms to resolve. This treatment preserves the uterus and potential fertility.
MR Guided Focused Ultrasound – A new, non-invasive, outpatient procedure that uses high doses of focused ultrasound waves to destroy uterine fibroids, without affecting the other tissues around the fibroid. The procedure is conducted in an MRI scanner which helps the physician "see" inside the body to guide and continuously monitor the treatment.
It is effective in single fibroid and depends on location of fibroid.
Q. Can Uterine Artery Embolization be used to treat other conditions such as uterine adenomyosis
A. UAE is also indicated for the symptoms caused by uterine adenomyosis with pain or abnormal bleeding.
Q. Is uterine fibroid embolization (non-surgical treatment) a safe procedure?
A. Uterine fibroid embolization has been performed safely in thousands and thousands women worldwide. While no procedure is without risk, fibroid embolization has been shown to have a lower major complication rate than traditional surgical treatment options such as myomectomy. The few potential complications are infection and ovarian failure leading to premature menopause. Infections are extremely uncommon and can usually be treated with oral or IV antibiotics. Rarely (much less than 0.5 percent), can develop and may require to undergo a hysterectomy. Ovarian failure leading to premature menopause is also relatively uncommon occurring in 1 percent of most patients who nearing menopause.
Q. What can I expect during the procedure?
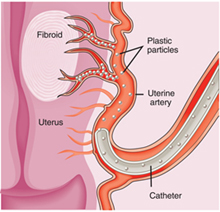
A. UTE requires an overnight stay in hospital. Prior to embolization, the patient will be sedated and remain drowsy throughout the procedure. Most procedures take approximately 20-30 minutes. An Interventional Radiologist performs the UFE through a small catheter inserted into the femoral artery in the groin. A local anesthetic is used to numb the skin and no stitches are needed after the procedure.
An X-ray is performed to give the doctor a clear picture of the blood supply to the uterus & fibroid using angiographic techniques, the catheter is guided through the artery to the uterus and tiny plastic particles are slowly injected into the arteries that supply blood to the fibroid. Over several minutes, these particles block the blood supply to the fibroids. With-out a blood supply, a fibroid will shrink up to 65-100%. The embolization is continued until the blockage of blood flow to the fibroids is complete. After complete embolization of one side is done, the other side is embolized. Though blood supply to the fibroids is blocked, arterial flow will remain to the normal of the uterus.
Q. What happens to the fibroids after embolization?
A. After UFE, the fibroids shrink and die while the normal uterus and uterine tissue lives.
Q. What happens to the small particles used during the UFE procedure?
A. The tiny particles used to block the blood supply in the uterine arteries are trapped within the small branches of the uterine arteries within the leftover fibroid tissue. They are too large to travel forward through the small capillary bed and they cannot move backwards in the uterine artery against the remaining incoming blood flow.
Q. Are there any types of fibroids that cannot be treated with UFE?
A. Most fibroids can be successfully treated using uterine fibroid embolization. Large fibroids can be considered as candidates for joint procedures using a combination of uterine fibroid embolization and laparoscopic myomectomy.
Q. Do fibroids grow back after UAE?
A. There is no evidence at this time that adequately treated fibroids grow back after uterine fibroid embolization. By comparison, approximately 30 percent of patients have a recurrence of fibroids after myomectomy.
Q. Will my insurance cover uterine fibroid embolization?
A. Most major insurance companies are now covering uterine fibroid embolization. Depending on your plan, specific referrals or other preauthorization may be necessary. Our clinical coordinator will assist you thru the approval process.
A. The uterine fibroid embolization procedure itself is painless. The only pain encountered by the patient is the local anesthetic shot at the puncture site near the right hip. For the pain reason, we keep patients overnight in the hospital for pain control. The morning after the procedure, the symptoms have usually improved to a point where they can be easily controlled with oral medications provided for the patient at the time of discharge to take home.
Q. How long until I can return to work after UAE?
The average recovery time before patients return to work or their normal daily activities is approximately one to three days.
Q. What type of follow-up is required after the UAE procedure?
A. After the procedure, we ask you to return to our office for routine follow-up in seven to 10 days. We also ask that you schedule an appointment to see your gynecologist in two to three months after the procedure for a routine gynecologic exam. We will plan for follow-up MRI in six to nine months to assess the results of embolization and to insure that the blood supply to the fibroids is eliminated.
A. While it varies significantly from hospital to hospital, in general, uterine fibroid embolization is less expensive to hysterectomy and myomectomy. In many areas, it is reported to be less expensive due to the shorter hospital stay and no need for general anesthesia.
Q. How successful is UAE in controlling symptoms caused by fibroids?
A. Heavy menstrual bleeding (menorrhagia) is controlled in 95-97 percent of patients after their procedure. Bulk related symptoms such as pelvic pain, pelvic pressure, frequent urination, constipation, back pain and painful intercourse are controlled in 95 percent of patients undergoing UFE.